WESTBOROUGH, MA August 3, 2015 Post-concussion Syndrome (PCS) effects about 5-10 percent of those who experience a concussion or mild traumatic brain injury. By definition it is diagnosed when patients fail to recover from their concussion in the expected 2-3 weeks or sometimes longer. This happens for a variety of reasons that are not always readily apparent. Sometimes the expectation of a quick recovery is thwarted by the return to full activity too soon, according to Michael Sefton, Ph.D Director of Neuropsychology at Whittier Rehabilitation Hospital in Westborough, MA. For example, when returning to work after 2-3 days of rest one should not expect the brain to be fully healed. As a result, a return-to-work plan is essential. Post concussion syndrome is not common but as many as 10-14 percent of cases exceed the usual 7-10 day recovery period.
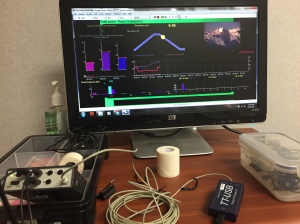
There are biofeedback protocols for post-concussion syndrome (PCS) that have been shown to improved the autonomic nervous system mismatch that often accompanies PCS. Here at Whittier Rehabilitation Hospital I have been using HRV entrainment to activate, or entrain the parasympathetic “braking” system that may directly lower the arousal associated with concussion including muscle tension, anxiety, elevated pulse, and suboptimal breathing. The method uses paced breathing for greater autonomic resonance and has been shown effective with pain management, poorly deployed attention, ADHD, and peak performance training.
Heart rate variability is a measure of cardiovascular health (Conder and Conder, 2014). A link has been demonstrated between traumatic brain injury, even concussion, and multiple organs including the heart (Cernak and Noble-Haeusslein, 2009). The effects of brain trauma impact structures deep within the brain including the brain stem. These cerebral regions impact cardiac function and can lead to cardiac illness.
People believe that the body’s autonomic nervous system can be thrown off after a concussion slowly becoming irregular resulting from an abnormal stress response. There is a deactivation of inhibitory neurons in the brain resulting in greater sympathetic activity. Thayer and Lane (2009) propose a right prefrontal cortex as having a direct role in cardiac modulation. This results in decreased heart rate variability and often increased heart rate and a host of other physiologic signs that prolong the recovery from concussion. Williams et al. (2013) proposed a white matter hypothesis highlighting the connection between white matter pathways in the brain and interaction between the amygdala and the sympathetic nervous system. Autonomic dysfunction is a well established underpinning of elevated stress. Hypertension is a leading cause of death around the world and may be attributed to the body’s abnormal response to external factors like stress.
“Traumatic brain injuries or TBI can occur at any time while working, playing, driving, or riding a bike! TBI is described as a public health problem that results from a sudden force being applied to the head and brain that results from high-speed acceleration-deceleration force coupled with secondary injuries from axonal shearing, cerebral edema, hypoxia, bleeding within the cranium, and autonomic dysfunction” (Sefton, 2014). In cases of brain injury one might see autonomic storming as just described that results from trauma to regions of the brain that control primitive bodily functions like respiration, heart rate, and emotional regulation.
“The brain stem regulates heart rate and respiratory drive as well. These functions are vital to survival and comprise the autonomic nervous system.” (Sefton, 2014) The human stress response drives a growing imbalance of the autonomic nervous system. Namely, the sympathetic nervous system, responsible for our innate fight-flight response is gradually accelerated adding to an influx of stress hormones like cortisol that can cause inflammation in the body. Cortisol can also have negative impact on sleep, memory, and acts as an appetite stimulant (APA). Scientists and physicians agree that chronic inflammation within the body can lead to failure in the affected systems like the heart.
Conder R. and Conder, A. (2014) Heart rate variability interventions for concussion and rehabilitation. Frontiers in Psychology, Review Article, August 2014, Volume 5.
American Psychological Association: cortisol. (n.d.). The American Heritage® Science Dictionary. Retrieved August 04, 2015, from Dictionary.com website: http://dictionary.reference.com/browse/cortisol
Sefton, M. (2014). Autonomic dysfunction: “Storming back from brain injury” Blog post. Retrieved August 6, 2015.
Thayer J. and Lane R. (2009). Claude Bernard and the heart-brain connection: further elaboration of a model of neurovisceral integration. Neuroscience Biobehavioral Review, 33, 81-88.
2 thoughts on “Heart rate variability: Biofeedback options for Post-concussion Syndrome”