The capacity for the eye-hand-brain to work in concert is called visuomotor functioning, spatial planning, and visual organization and processing. The capacity to see things as they are and to understand them belies the cognitive component involved with driving a motor vehicle. When driving a car, operators are expected to be alert, have full field of vision, and preserved capacity to make quick and easy decisions. Some of our driving acuity begins to change as our attention and speed of processing wane. As we age sensory input changes. I often encourage family members to have a driving evaluation when negotiating over who should drive. These lessons take the decision over who is a safe drive away from a husband or wife placing it on the driving instructor. After a stroke, it is possible to regain driving privileges but the driving evaluation with a driving school it takes the decision away from family members.
Neuropsychology
South African boxer Simiso Buthelezi dies from brain injury: grotesque ending bout punching ‘invisible opponent’ in Durban

This is a tragic ending to a young man’s career. Simiso Buthelezi died hours after a title match in South Africa. The 24-year-old faced compatriot Siphesihle Mntungwa for the WBF All Africa lightweight title on Sunday June 6, “but the 10-round contest was stopped by the referee after Buthelezi appeared to shadow box an invisible opponent” according to South African news in Durban. Shortly after exhibiting a “grotesque display of confused pugilism”, the referee stopped the fight. Buthelezi could no longer discern or process his environment and collapsed. He suffered brain herniation from rapid swelling and bleeding within the skull know at second impact syndrome a rare condition that results from repeat blows to the head. It is often fatal. This man died two days later. The fight is published on You Tube. This should not have happened. Simiso should be alive today but these fights are sanctioned and go on across the world. No sport should sanction that the best way to win is to render your opponent unconscious. Does anyone still doubt that brain injury may be the likely outcome from MMA fighting and bare knuckle BKFC sanctioned street fighting? We learned the risks from microscopic analysis of the brains of deceased athletes in the National Football League a decade ago. These injuries are still finding their way to media reports as athletes die in retirement. Recently it was published that the average life expectancy of an NFL athlete is 59.7 years. Here in Boston, the Boston University Legacy Brain Bank has examined hundreds of brains of athletes who have died. Chronic Traumatic Encephalopathy (CTE) results from repetitive blows to the head that gradually steal brain function and exhibit a host of radical emotional and behavioral changes. Are the South African WBF unfamiliar with these studies? And in Philadelphia, the Bare Knuckle Fight Club is contracting with athletes to fight without gloves in a violent, barbaric display of street justice.
Mntungwa was the one who was knocked through the ropes prior to the incident, which confused doctors as Buthelezi landed the more damaging blows in the contest. They now fear Buthelezi may have entered the ring with a pre-existing injury having been minutes away from a comfortable victory.
Ben Davies Mirror 10 June, 2022
Both 2021 and 2022 have been deadly years for traumatic brain injuries among Mixed Martial Art (MMA) fighters and now the bare knuckle fighters who are often men and women who fight without gloves and are the barbaric street fighters who risk their lives each time they step into the ring. Fights like these were mostly unsanctioned and underground events, akin to cock fighting where patrons bet money on who might kill his opponent. This is not a new problem. Boxer Mike Trowell (shown below) left a family behind when he died after a blow to the head during a bout in Scotland in 2016. Trowell died shortly after a fight in Glasgow on September 30, 2016. He was knocked down in the first round and visibly injured. After a standing 8 count, he was allowed to continue the fight. He was again knocked down in the fifth round. At this point, he became unresponsive and was transported to the trauma center where he died after being removed from life support. Mike Trowell had been having severe headaches for days before his final fight and should never have stepped foot in the ring.

Brain bleeds can occur when the brain collides with the inner side of the skull. I have discussed these emergencies many times on the pages of this blog. The violent collision from gloved fist striking the head of an opponent may cause tears in blood vessels within the skull and intracranial bleeding. Athletes never expect this to happen to them. This injury results in pools of blood forming between the brain and the skull. We know there is not much extra space in the skull surrounding the brain matter. There are now fighters in Mixed Martial Arts and Bare Knuckle (BKFC) fighting that are ultra violent and most anything is fare game. Once blood collects in the convolutions of the brain it does not drain easily resulting in brain swelling and unconsciousness. The build-up of blood will cause pressure on the brain which leads to seizures, coma and often proves fatal.
Mntungwa returned to his feet and was ready to resume the fight when Buthelezi seemed to lose his bearings. The fighter’s first instinct was to bear down as though the referee was his target, only to then move into the corner and start throwing fists as though shadow boxing.
In October 2021, bare knuckle fighter Justin Thornton died after being knocked out in the first round of a BKFC battle in Mississippi – an off shoot of the MMA. These fights are essentially street brawls and bear no resemblance to the pageantry of boxing. Bare Knuckle Fighting Championship (BKFC) is the first promotion allowed to hold a legal, sanctioned, and regulated bare knuckle event in the United States since 1889, according to the BKFC website. I would be surprised if any physician would sign on to provide care to the victims of this savage form of entertainment. In Massachusetts, MMA fighter Christian Lubenga died 2 days after a devastating blow to the head following a fight at the AMMO Fight League: Battle of St. Patrick’s event on March 12. The event was held at the Eastern States Exposition in West Springfield, MA. Lubenga wrote that he was a grad student, a father and someone who was “martial arts addicted”. He also expressed his dream to become the “next Congolese UFC champ” taken from Lubenga’s social media presence and reported in MMA Health and Science news.

Any man or woman who steps in the ring or the cage is special, they take a risk that 99.99% of the world would never take and sometimes, I still don’t know why we do it … but Justin was a fighter his entire life and deserves nothing but respect!
Dillon Cleckler – Justin Thornton’s opponent in his final fight
This is not a male-only fight problem in Mixed Martial Arts. During 2021, an 18-year old girl died following a 4th round knock out in a sanctioned fight. Mexican-born Jeanette Zacarias-Zapata faced Marie-Pier Houle in a pro boxing bout at the IGA stadium in Montreal, Quebec, Canada. Jeanette Zacarias-Zapada was married and travelled to Montreal for her debut fight. After sustaining a number of blows to the head, at the close of round four, Jeanette was unable to return to her corner and the match was stopped. At this point, her life was held in the balance suggesting a true neurological emergency. Next, she had a grand mal seizure – an ominous sign that the brain was awash in blood from the violent blows tearing brain tissue and vessels in the brain. She was then transported to the trauma center in Montreal and died with her husband at bedside. The risk – reward conundrum: whether to risk a rare bleeding in the brain after repeated violent punches to the head or win the match and the accolades that come from being in the winners corner at the end? For some who desire to achieve greatness in their sport and recognition in their country it is an easy answer.
NFL football, as well as other major sports here in America, have well established protocols to look at the impact of cumulative trauma to the brain and normal brain functioning. For the most part, athletes know what is expected of them when they experience a blow to the head with any alteration in their cognitive functioning based on the examination by the athletic trainer and the team physician. The NFL has spotters high above the field to report any player who may be altered due to a blow to the head. When this occurs play is stopped and these athletes are quickly removed. Some try to outsmart the medical staff by cheating on post-injury concussion testing. Especially on the sideline. At one point during a presentation to high school athletes and their parents, a school employee made the comment that when he played varsity football, for this same school, he was returned to play twice after being rendered unconscious during a football game. He was articulate and well spoken and served as the school’s custodian.
In recent years, athletes have donated their brains to the Boston University post mortem brain study that looks at the impact of an NFL career on brain health including: repeated concussions and the brains athletes who have not received any clinical diagnosis of concussion but may feel they have changes in their thinking and emotional regulation. The brains undergo post-mortem microscopic analysis to look for tell tale signs of chronic traumatic encephalopathy (CTE). Am I the only one who sees the value of these studies?
While this collection of brains is not perfect and they are often inconclusive as to the presence of CTE. Meanwhile, athletes are getting better medical care and are assessed soon after the injury before being allowed to return to play, whenever possible. This is referred to as “the concussion protocol”. The protocol is designed to avoid the potential for a catastrophic second impact syndrome that has the potential to quickly render an athlete permanently disabled and has a high degree of fatal outcomes. This was not the case, nor the protocol, in the 70’s, 80’s, 90’s as a literature on CTE has shown. I’ve written about this tragic outcome in prior publications here and on the Human Behavior blog, as well as in case consultation with Robert Cantu, MD at Boston University Medical Center, with whom I’ve consulted on several cases, and Michael Collins, Ph.D., with whom I spent time in practicum at the University of Pittsburgh Medical Center concussion clinic in Sports Medicine. Dr Collins is very open with is time and deserves many thanks for his timely supervision for those of us that were learning about concussion years ago.
While this collection of brains is not perfect, they are often inconclusive as to the presence of CTE. Meanwhile athletes are getting better medical care and are assessed soon after the injury before being allowed to return to play, whenever possible. This avoids the potential for a catastrophic second impact syndrome that has the potential to quickly render an athlete permanently disabled and has a high degree of fatal outcomes.

The trend in cognitive stability quickly changed for longer-tenured fighters, in whom the research team repeatedly observed significantly higher-than-normal brain volume loss, which is a key culprit behind diminished brain function and typically is caused by aging, disease or trauma. Athlete’s C-T scan following a TKO during MMA battle – note apparent frontal and frontoparietal lesions
Scot Harris, 2013
I often wonder if people react to the current fight club – MMA matches with any sort of concern for the men and women who are paid a paltry sum of money to enter the ring with the sole purpose of giving their opponent a brain injury from which they may never recover?
Repetitive impact now 10 years on: MMA and its fierce defiance of brain trauma and sometimes fatal impact on athlete well-being

NFL football, as well as the other major sports, have begun to take a serious look at the impact of cumulative trauma to the brain. This isn’t new. Remember, Will Smith as Dr. Bennet Omalu, the pathologist who made the initial discovery of chronic plaques and the build-up of of tau protein that can lead to apoptosis – programmed cell death. In 2016, I first wrote about the topic of sports-related concussion and its treatment and was initially studying brain injury in 1992 at La Palma Intercommunity Hospital in the Los Angeles area.
In recent years athletes have donated their brains to the Boston University post mortem brain study that looks at the impact of an NFL career including recurring concussions. And to some extent, those that have not received any diagnosed concussions during their careers. While it’s not perfect, athletes are getting better medical care and are assessed carefully before being allowed to return to play, whenever necessary. This was not the case, nor the protocol, in the 70’s, 80’s, 90’s as the literature on chronic traumatic encephalopathy he began to slowly grow. I’ve written about this in prior publications as well as in case consultation with Robert Cantu, MD at Boston University Medical Center, with whom I’ve consulted, and Michael Collins, PhD with whom I spent time in practicum at the University of Pittsburgh Medical Center concussion clinic.
Indeed, if the major sports are now developing protocols that includes removing athlete from play, it seems ironic that mixed martial arts MMA – has failed to establish a routine protocol that protects athletes from repeated, uncontrolled, and violent, bare fisted blows to the head especially when an athlete has been rendered unconscious and is unable to protect himself or herself. Am I the only one who notices this reckless pattern only to have a referee break up the bout after 5-10 head strikes once the opponent goes down. Defenseless! This often includes head kicks as well. Am I the only one who refuses to endorse this as nothing more than a glorified street brawl? Why hasn’t Dr. Cantu at BUMC or Dr Collins in Pittsburgh taken more of a stand speaking out about this spo
The Brain’s inflammatory response from Neurosarcoidosis

This paper is about neurosarcoidosis an inflammatory condition in the brain. It can be the source of “focal neurology, multifocal neurology or diffuse encephalopathy due to parenchymal lesions of the brain or brainstem” (Ibitoye, et.al. 2017). Optic neuopathy is a common sequelae of neurosarcoidosis as a result of its impact from inflammatory dysregulation and the real estate taken up by optic nerve and its projections. Other “common presentations included cranial nerve palsies, spinal cord and brainstem manifestations” (Zajicek, et.al. 1999). Another in a series of conditions that may be autoimmune-related and very detrimental to neurocognitive functioning. Most cases of neurosarcoidosis also have been treated for sarcoidosis in another organ system which I describe later. I am most interested in the evolution of neurosarcoidosis and sarcoid meningitis. Neurosarcoidosis is a “cryptogenic neuroinflammatory diseases, neurosarcoidosis should be considered after excluding common infections and autoimmune causes”(Mubarik, et.al. 2018).
DEFINITION: Cryptogenic neuroinflammatory disease is largely obscure and often difficult to diagnose and establish a definitive etiology. It is often a diagnosis of exclusion.
Merriam-Webster Medical Dictionary
Sarcoidosis is a condition that results from an inflammatory response affecting the organ systems in the human body. Lungs, liver, lymph system, kidney and more rarely, the brain. Sarcoidosis is among the conditions we sometimes see at Whittier Rehabilitation Hospital here in Massachusetts. They are rare conditions that produce masses or nodules called granulomas in the affected organ systems. These are very difficult to control. It is more common in females and generally hits between 20-40 years of age. The incidence of new cases is 4 in 10,000.

Sarcoidosis is an autoimmune disorder by most accounts. It can be remitting in that the granulomas are small and do not impact the affected organ system like the lungs or kidneys. The granulomas are actually groups of immune cells that form a single mass or a cluster that becomes attached to the lung, kidney, lymph node, etc. The US Department of Health and Human Services reports that most individuals will recover and go on to have normal lives. The NIH National Heart Lung and Blood Institute reports that sarcoidosis may be triggered by infection and perhaps environmental exposure. This is why firefighters may be at higher risk for acquiring the disease. Imaging studies like x-ray, C-T Scan, VQ nuclear medicine scan, and MRI provide the definitive diagnosis.
Web MD lists these common complaints of patients experiencing the effects of sarcoidosis. Initially patients complain of a persistent dry cough, fatigue, and shortness of breath. Other symptoms may include:
- Tender reddish bumps or patches on the skin.
- Red and teary eyes or blurred vision.
- Swollen and painful joints.
- Enlarged and tender lymph glands in the neck, armpits, and groin.
- Enlarged lymph glands in the chest and around the lungs.
- Hoarse voice.
- Pain in the hands, feet, or other bony areas due to the formation of cysts (an abnormal sac-like growth) in bones.
- Kidney stone formation.
- Enlarged liver.
- Development of abnormal or missed heart beats (arrhythmias), inflammation of the covering of the heart (pericarditis), or heart failure.
- Nervous system effects, including hearing loss, meningitis, seizures, or psychiatric disorders (for example, dementia, depression, psychosis).
The WRH case presentation of Mr GR. GR is a 66-year old male with liver cirrhosis due to sarcoidosis. He was diagnosed with sarcoidosis over 20 years ago. On admission to our hospital, he was identified with left-sided weakness, saccadic movement abnormalities (rapid saccadic movements and some occular bobbing during EOM testing), no nystagmus, upper extremity ataxia, and dysmetria. Rheumatology and Infectious Disease consults were obtained and it was thought the patient was suffering from neurosarcoidosis. Opthalmology diagnosed blepharitis. A cerebellar lesion was seen on brain imaging, possibly neurosarcoidosis which was supported by elevated serum ACE. This is usually established via a lumbar puncture. GR was treated with high dose steroids with improvement of his symptoms and transferred to WRH for physical rehabilitation.
The Zajicek criteria cited lesions involving brainstem and/or cerebellar presentations occurred in 14 patients (21%) who principally exhibited limb or gait ataxia and eye movement abnormalities such as failure of vertical gaze. Mr R. underwent an MRI brain which that showed T2 flair hyperintensity in the cerebellar vermis and left dentate nucleus – that had also been previously seen on October 2020 imaging. There were chronic microangiopathic changes suggestive diffuse damage to white matter pathways.

Mental status: Alert and oriented x 3. Able to provide reliable history. Able to name low frequency objects. Able to repeat. Able to follow complex command. Able to spell radio forwards, but not backwards. *NOTE: more formal neuropsychological testing did identify other cognitive deficits.
Mood/affect: Denies overt depression. States mood is stable. Affect euthymic. Speech/language: speech is both dysarthric as well as scanning. There is some delay and hesitancy in speech that may be misinterpreted as confusion – though in our encounter the content of his speech was accurate and reasonable.
Cranial nerve testing was done: Pupils 3 mm round, equal, reactive to light. Visual fields full to confrontational testing. He had difficulty maintaining primary gaze as there are saccadic intrusions. With horizontal eye movements, there is breakdown of smooth pursuit. Facial sensation is intact and equal. Face is grossly symmetric (though has a beard). Hearing is intact and equal bilaterally. Tongue and uvula midline. Shoulder shrug was equal. There were no abnormal movements at rest. Bulk and tone are normal. Full strength throughout.
Overall cognitive findings reveal significant deficits in immediate and delayed memory, visuospatial processing, attention, language, and speed of processing. For example, on the verbal Semantic Fluency subtest, R. has difficulty getting into set and was unable to name any fruits or vegetables as the task required, instead resorting to naming different types of pasta. Further visual motor testing was administered with the Cancellation tests and was again completed at a slow speed – there was no particular visual field deficit or obvious neglect. Of note, the RBANS List Learning subtest was completed separately on early in the hospital stay. Further visual motor testing was initiated in the setting of slow speed of executing visual motor tasks. He is quite dysgraphic on tests of written language. He has lost his personal signature. On the Luria Patterns test, he executed the design with noted perseveration. The clock drawing was completed with errors in numeric and hand placement with the same slow speed of processing. He is grossly oriented and aware of the circumstances leading up to this hospitalization and has fluctuation in his level of cognitive functioning. He had significant deficits in working memory and attention.
___________________________________________________
Ibitoye, RA., Scolding, WN, Scolding J. (2017) J Neurol; Neurosarcoidosis: a clinical approach to diagnosis and management, 264(5): 1023–1028. Published online 2016 Nov 22. doi: 10.1007/s00415-016-8336-4PMCID: PMC5413520 Taken 11-16-2020
Zajicek JP, Scolding NJ, Foster O, Rovaris M, Evanson J, Moseley IF, Scadding JW, Thompson EJ, Chamoun V, Miller DH, McDonald WI, Mitchell. (1999) Central nervous system sarcoidosis–diagnosis and management. DQJM. Feb; 92(2):103-17.
Mubarik, A Hassan, SM Hassan, Felix, M, Muddassir, S, Haq, F. (2018) A confusing manifestation: a case report of neurosarcoidosis presenting with confusion. J Community Hosp Intern Med Perspect. 8(6): 363–367. Published online 2018 Dec 11. doi: 10.1080/20009666.2018.1536239PMCID: PMC6292345
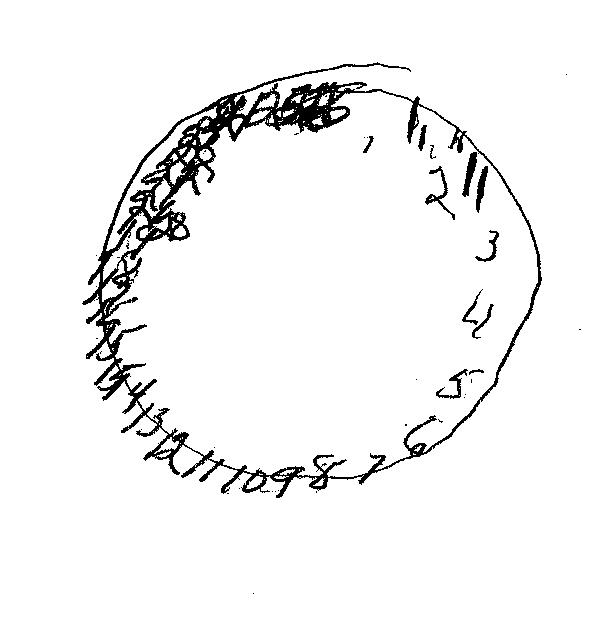
Clock of the Week: Summer 2020

The Clock of the Week for late August 2020 is drawn by a 57- year male who is undergoing acute rehabilitation for liver failure. He is awaiting a liver transplantation and in recent weeks has become increasingly confused. This task requires linguistic understanding and the capacity to retain a 3-step command.
The patient is suffering from hepatic encephalopathy which results from a build-up of toxic, metabolic substances in the blood that are typically removed by the functioning liver. If you have a particularly interesting clock, feel free to send it along to the email address listed in these pages.
Memory testing to rule out dementia: Step one is simple
This is a simple test developed by M. Marsel Mesulam, MD, first published in Behavioral Neurology textbook in the early to mid 1980’s. Mesulam was a great teacher and his posit was that the left hemisphere processed the linguistic (verbal) material while the right hemisphere processed the abstract (design) stimuli. This may be thought of as the first step of the cognitive assessment of memory and is useful to rule out: alexia, agraphia, and aphasia. It is a perfunctory test and often turns out normal – rate of false negative higher than false positives. The instructions are simple: “I want you to copy all that you see here in front of you.” Watch what this person does with these basic instructions.
Immediate cognitive awareness: impact on ADL’s
A cognitive task for him to ask for the ages
Here is a video that was taken recently with a patient who is having  difficulty understanding directions, and his speed of processing is quite slow. You’ll see in this video a patient struggling to integrate and understand the directions of the task even though they are quite simple. The clock drawing and other cognitive measures such as the three shapes, three words, memory test, and the line by section test, reflect and illustrate the difficulty in cognitive processing following either a traumatic injury to the brain, or some declining, progressive cognitive impairment associated with dementia dementia of the Alzheimer’s type, vascular dementia, and others.
Cognitive Assessment and driving
Perseveration refers to the repetition of a behavior that exceeds the demand such as the repetition of lines or circles beyond the modeled current stimuli.
Visual Motor tasks
Here is one of the assessments I conduct daily, of an older client who has changed cognition due to dementia. It is sad to see the decline of personal awareness and inhibitory control. This man had minimal awareness of his preservation and became “stuck” in set.


Assessment of Basic Memory – 3 Shapes 3-Words remembering Mesulam
Here is a magnificent video from a neuropsychological assessment of a patient at Whittier Rehabilitation Hospital. It depicts the impact of changes in neurocognitive functioning and the response of the brain to illness, whatever that may be. The test is a screening tool developed in the 1980’s by M. Marsel Mesulam, MD who wrote text book Principles of Behavioral and Cognitive Neurology when on the faculty at Harvard Medical School. He was the driving force of the annual Behavioral Neurology course offered by Harvard Medical School. He has since moved his practice and the course as well to the Feinberg School of Medicine at Northwestern University. The book is well worth having in your personal library. The Three-shapes Three-words Memory screening is a useful tool, and provides some interesting data, upon which one might make assumptions on the laterality of patient deficits that are rendered.
It was proposed that the shapes were processed by the non-dominant right hemisphere, while the words were processed and encoded by the dominant left hemisphere. Deficits in one or the other might represent the lesion underpinning the laterality of the findings. So if the words were poorly executed, and quickly forgotten than one might anticipate a lesion on the left in the middle cerebral artery, preps along the arcuate fasciculus, whereas a lesion on the right, might reveal signs of poorly executed designs, and a lack of recall of the abstract stimuli, thought to have been processed by the right hemisphere, recovering from cerebrovascular accident, or some other underlying neurocognitive deficit. This assumption certainly requires some secondary neuropsychological testing, which is done to assess the functioning of both sides of the brain and certainly the bundle of fibers connecting the two.
Speed of Processing and changing cognitive efficiency
Here is a video of a recent neurocognitive screening that includes visual motor functions. Whittier Rehabilitation Hospital takes care of patients with brain injury, stroke, dementia, and a complete orthopedic service. It is one part of the neuropsychological assessment. This screening is among the first activities I do when meeting a person. It tends to be well accepted and engaging. Out of respect for the patient we start with things that should be easy such as writing short sentences, copying designs, and drawing a clock. Clock drawings are often reported in these blog pages. The neurological underpinning for these are multifactorial. But using the deficit model of error detection is useful to make assumptions about localization of brain damage. It is not always possible to pinpoint where in the brain a lesion may be located. In fact, the use of MRI and functional MRI (fMRI) are far more accurate in localization of a suspected lesion. However, the localization of the lesion is one substrate associated with the functional changes observed in patient data and behavior. This is important to assess because there are several conditions that impact speed of processing, including traumatic brain injury, altered mental status due to encephalopathy, and progressive conditions like MS, Parkinson’s Disease, and the dementias. What we’re looking for in this case is the efficiency by which the patient can switch cognitive sets and go from one task to another. It is also interesting to see how long this person takes to process the directions and can she process more than one set of directions at a time and work in parallel with her cognitive processes. After the clock drawing, I sometimes add a bicycle drawing and line bisection test, and a test of continuous performance used to measure concentration and sustained attention. Some people complete the CPT with 30 seconds to one minute of sustained attention but it is recommended that clinicians complete 2-4 minutes of continuous responding for greater accuracy.
First blood and now saliva testing for concussion: it is about time!
The diagnosis of concussion has been a tenuous one from the beginning because some believe that loss of consciousness is the definitive sign of have one’s bell rung. Over and over, I have challenged the myth that loss of consciousness is the sine qua non of concussive injury. Not so fast. There is a high degree of false negative findings in these, meaning that the test may not reveal the cerebral reverberations left by a blow to the head. Especially sports like rugby, ice hockey, and American football. I have also written about the mixed martial arts and kick boxing now accounting for significant traumatic brain injuries and death.
It has been en accepted fact that one need not lose consciousness to be considered to have sustained a concussion. Anything, from sitting up too quickly in a low hanging bunk bed to having a loose basketball strike during a shoot around can result in symptoms. We remember, concussion is defined as any force to the head sufficient to cause alteration of brain functioning. Symptoms such as confusion, slow speed of processing, headache, loss of memory, sleep disturbance, depression, sensitivity to light and sound, and even nausea. There are more symptoms when you look at the CDC website devoted to concussion but the ones listed are prominent among the patients I follow. Residual headaches and fatigue seem to be most recent and long lasting.
Dr Matt Cross, head of Science and Medical Operations at Premiership Rugby, said, “We would like to thank our clubs and all of the players for volunteering to be part of this very important research project. The findings from the study are clearly promising and highlight the potential for salivary biomarkers to further support clinical decision making and the accurate identification and diagnosis of concussion in a range of different sporting and non-sporting settings.”