The capacity for the eye-hand-brain to work in concert is called visuomotor functioning, spatial planning, and visual organization and processing. The capacity to see things as they are and to understand them belies the cognitive component involved with driving a motor vehicle. When driving a car, operators are expected to be alert, have full field of vision, and preserved capacity to make quick and easy decisions. Some of our driving acuity begins to change as our attention and speed of processing wane. As we age sensory input changes. I often encourage family members to have a driving evaluation when negotiating over who should drive. These lessons take the decision over who is a safe drive away from a husband or wife placing it on the driving instructor. After a stroke, it is possible to regain driving privileges but the driving evaluation with a driving school it takes the decision away from family members.
Category: Human behavior
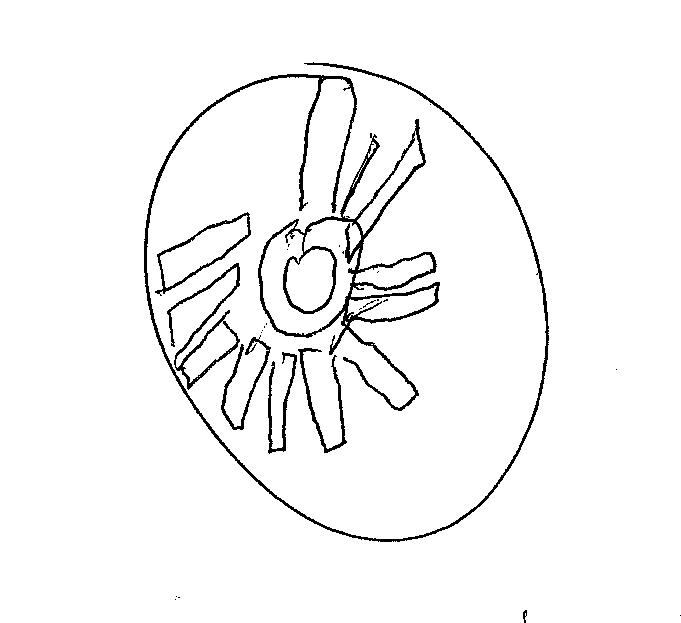
Clock of the Week August 5, 2021

The clock of the week has the flavor of someone having a difficult time executing the basic 3-step command. It is quite grand in its elaborateness and the time it took create this clock was extensive. Speaking all the time while drawing, this patient is having the cognitive sequelae from the coronavirus. These long haul patients experience a host of neurocognitive underpinnings including poorly deployed attention, decreased speed of processing, fatigue, and decreased problem solving and self-monitoring. There are cases we are following here at WRH with significant memory-learning deficits – well below baselines. Others are exhibiting decreased cognitive efficiency and mental slowing. What to do?
Recovery has been estimated in weeks to months from onset. Continued speech language pathology and neuropsychological support are essential. Psychotherapy is important for those who experienced trauma-related exposure. A specific return-to-work protocol should be tailored for each discharging patient. A job analysis must be undertaken during the on-going treatment and sometimes parceled out for safety and efficiency. Job mentoring is useful as well. Readers are reminded that many people who may have had the virus in early or mid 2020 can have a return of symptoms or lingering symptoms that may be quite debilitating. Call us here at Whittier Rehabilitation Hospital in Westborough for teaching, consultation, and treatment from this pandemic-related problem. Outpatient Service 508-871-2077 in Westborough, MA
Coronavirus and long-haul “brain fog” similar to that reported in post-concussion syndrome

Much like lingering symptoms of concussion, a condition know as post-concussion syndrome or PCS, patients who are covid-recovered are starting to complain of “brain fog” weeks even months after recovering from the virus. Patients with PSC often describe having problems with mental endurance, decreased processing speed and efficiency that leave them feeling “in a fog”. So too are patients who have been through the coronavirus, even those who have had minor symptoms and over half who have never been hospitalized with severe virus. In fact, the most sick, those who spent time on a ventilator actually faired the best in a recent study from Italy.
The patients with severe COVID-19 experienced multidimensional functional deficits in mobility, cognition, speech, and swallowing which were pervasive at the time of admission to rehabilitation.
Michael Sefton
Stages of Coronavirus Infection
Stage I Damage to nervous system was initially thought to be limited to the epithelial cells in the nose and mouth – hence the loss of smell (41 %) and taste (55 %). These were individuals who may have experienced slight flu-like symptoms or may have thought they had a bad cold. Most were not tested for coronavirus in the first wave in early 2020 (JAMA Head & Neck 2020).
Stage II As the virus triggers an inflammatory response it can lead to the formation of clots anywhere in the body which can cause pulmonary emboli and strokes. In this pulmonary phase the immune system becomes strongly affected by infection and leads to primarily respiratory symptoms such as persistent cough, shortness of breath, and low oxygen levels. It has been observed that at this point patients can fail very quickly.
Stage III There is a huge viral load that results in an explosive inflammatory response called a cytokine storm. This impacts all body systems including lungs and heart. It can damage blood-brain barrier allowing inflammatory cells and perhaps viral particles to enter the brain – which can lead to seizures, confusion, coma, encephalopathy. Essentially this is a runaway immune response.
As I have described in the Word Press Human Behavior blog people are reporting feeling cloudy and unfocused describing it as brain fog. I have heard the same description from people who are referred for concussion management as well following unresolved symptoms of concussion. Remember concussions do not require that the patient be rendered unconscious by the injury. Even mild traumatic force from a fall can leave someone in a foggy state for weeks. Recovery from second or third concussions are never the same. Similarly the cognitive effects of the coronavirus can be debilitating to 30-50% of cases. Here in the US there have been 32 million cases of coronavirus so the means as much as 16 million people may have some form of cognitive deficiency due to their infection. What does this mean for those of us offering treatment for cognitive-behavioral problems in general?
Like PCS, the virus impacts broad cognitive systems like attention, memory, and problem solving. Physical symptoms include shortness of breath, fatigue, and limited endurance. Whether it is a professional, elite student athlete or a salesman injured in a car crash there is an experience of stigma associated with the invisible injury of concussion and PCS. The emotional impact of this marginalizes patients often leaving them feeling alone and frustrated. This isolation and loss is shared by long-haul covid recovered patients.
Experience shows most long-haulers tend to fall into the high risk category, such as those with chronic respiratory disease such as COPD or multiple conditions including diabetes mellitus and obesity. But there is a growing percentage of people who were otherwise healthy before they became infected and are suffering with the same negative cognitive impact (Ferrucci, 2021).
Ferrucci reported on a small sample of cases that were hospitalized but not in an ICU. These finding were subjectively reported 4-5 months following their diagnoses.
31.6% reported cognitive decline
50% moderate to severe increased fatiguability
26.7% moderate to severe increased forgetfulness & lack of concentration
23.3% moderate to severe increased time to perform tasks such as reading/writing
20% moderate to severe difficulties in new learning
16% depressed mood
42.1% processing speed deficits
Formal neuropsychological testing revealed cognitive deficits in the following areas using the Repeatable Battery for the Assessment of Neuropsychological Status. Data reported below are from a small sample hospitalized in Milan, Italy.
26.3% delayed verbal recall
10.5% immediate verbal recall
18.4% impaired visual L-T memory
15.8% visual S-T memory
7.9% semantic verbal fluency deficits
As part of our review, in anticipation of questions we might get at the recent webinar, colleague Lauren Guenon and I learned that aggressive treatment is needed to assure that the patients who are returning to work are properly prepared. Recent peer reviews suggest having restorative physical and cognitive therapy 3-4 times per week. It is not clear yet whether Medicare will permit this intensity of service foe those recovering from coronavirus. Heading back to work too early can create set backs. We have also seen reported set backs that describe a return of respiratory symptoms and other signs of an errant and unpredictable inflammatory response. A gradual transition back to work is essential to insure a successful return to work. I usually prescribe a 3-4 week transition and make an effort to work with employers so they understand the importance of a staged work re-entry. I have not had an employer refuse a transition plan and most have offered their assistance returning the employee to service.
Ferrucci, R et al. (2021) Brain Sci. 2021, 11, 235.
Amjad H. Roth DL, Samus QM, Yasar S, Wolff JL. (2016) Potentially unsafe activities and living conditions of older adults with dementia. Journal Am Geriatric Soc. 64(6):1223-1232
Budson, A. (2020) B.U.Medical School — https://www.health.harvard.edu/blog/author/abudson
Gallagher, M, et al. (2020) The Impact of Covid-19 Experiences and Associated Stress on Anxiety, Depression, and Functional Impairment in American Adults. Cognitive Therapy and Research. https://doi.org/10.1007/s10608-020-10143-y.https://doi.org/10.1007/s10608-020-10143-y. Springer Science.
Goodman-Casanova JM, et al. (2020) Telehealth home support during Covid-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: survey study. Journal Med Internet Res. 22(5):e19434.
Sefton, M (2021) Long-haul symptoms of Coronavirus. Blog post https://msefton.blog/2021/06/26/long-haul-cognitive-effects-of-covid-19-in-those-who-have-recovered/ Taken 6/27/2021
Heneka et al. (2020) Alzheimer’s Research & Therapy. Long and Short-term Cognitive Impact of Coronavirus. 12:69 https://doi.org/10.1186/s13195-020-00640-3
Lawton, MP, Brody, EM. (1969). Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 9(3): 179-186.
Cognitive changes from Covid-19 pandemic infection can impact problem solving
The Coronavirus has impacted over 32 million Americans and has taken the lives of over a half million people in the past 14 months. Now, as people are getting fully vaccinated people in the physical rehabilitation field are finding that the long-haul cases who are considered Covid-recovered are suffering from a number of serious neurocognitive deficits that were unexpected
As you can see from the video above changes and cognition directly impact problem-solving, reasoning, and even something as simple as written language. We have seen in the studies that are published that the coronavirus pandemic has left many cases of long-haul cognitive change following infection. I have published blog posts across greater than five years of the impact of cognitive change including dementia, on the ability to follow a simple three-step command.
It was first thought to be primarily a respiratory disease and people who were older who had pre-existing pulmonary conditions might be most effected or most likely to die from the virus. We now see that in addition to loss of smell and taste there are a host of cognitive symptoms that have potential impact on the long haul cases into the future.
Since my training at Boston City Hospital – now Boston University Medical Center, I have learned that even simple tasks like drawing a clock result from subtle changes in cognition. Cognition refers to concentration, sustained attention and processing, memory and learning. These are things that we take for granted and often slip from our grasp prior to our conscious awareness of the loss. In other cases, the loss of appreciation for our cognitive strengths and weaknesses is insidious often noticed by our families only. The Covid-19 has rendered as much as 50 percent of survivors with the negative cognitive impact of something like a moderate traumatic brain injury.
Indeed, there are cognitive changes associated with the aging process. But higher order tasks of activities of daily living such as paying bills, driving, and something more complex like selling a home demands decision-making. Deficits in these mental functions may linger as a result of exposure to the coronavirus. This has a significant implication for individuals who want to head back to work.
Colleagues and I are seeing cases at Whittier Rehabilitation Hospital where patients who are admitted having recovered from the coronavirus are exhibiting lingering physical and cognitive changes that were not present prior to contracting the disease. Studies that are being published from the first wave in the Italian population of survivors reveal problems with fatigue as well as cognitive problems in concentration, mental acuity, speed of processing, and short term memory. They are peer-reviewed but small in their sample size between 9 and 50 cases each. Understanding this, we decided to look at a sample of greater than 72 recovering patients from the second wave here in New England.
The researchers examined patients admitted during the first surge of COVID-19 during Spring 2020. The study’s 29 patients were 70 percent male and 58.6 percent white, with a mean age of 59.5. The mean length of acute hospitalization was 32.2 days with a mean of 18.7 days intubated. Patients spent a mean of 16.7 days in inpatient rehabilitation, and 90 percent were discharged to their homes. Patients demonstrated significant improvement from admission to discharge in measures of fall risk, endurance, gait speed, mobility, cognition, speech, and swallowing.
Human stress and the uncertainty of Covid-19
In many posts I have espoused the need to managed stress. Some people are able to endure extreme levels of stress with little to no outward sign of distress while others boil over at the first sign of conflict or emotional ripple according to MSefton blog post. It is unavoidable in life but most of us need the occasional cue to lower our level of stress to health levels. Maybe this is when you have your annual check-up and you physician says you have gained 15 pounds since your last exam. Or perhaps your wake-up call comes when you are told your blood pressure is over 150 systolic. That’s not so bad right? And finally, your wake-up call may not come until you find yourself in an ICU after undergoing a lifesaving cardiac stent procedure after you experienced chest tightness while eating out with your spouse. In children, stress comes out as changes in normal coping behavior. Now, all bets are off and as a psychologist I am trying to offers matter-of-fact methods of keeping your stress in check.
Childhood stress reactions depend upon the developmental stage of the child. A younger child may become more clingy and fearful when feeling stress. They may cry more than usual and regress to earlier “safe” behaviors like wanting to sleep with a parent. Adolescents may be particularly more irritable and defiant as a way of regaining some control in their lives. They are now told “you have to stay home.” So-called social distancing does not resonate with the average invincible teenager. A recipe for percolating angst and loneliness. Many are using laptop computers for face-to-face social chats and this can help greatly. No every child has access to the internet and not all can utilize video platforms to access their friends. Students who are developmental challenged with autism often have few friends to whom they can reach out. Some parents set up video chat times with teachers or willing classmates but these often turn out awkward and contrived. The question we hear from kids – even adult children is when will it all end. Sports are a great source of stress relief for kids and their parents. Even though most collegiate, high school, and youth sports are on hold for the spring season exercise is an important way to reduce feelings of tension, anxiety, and pent up feelings.
“A marathon is 26 plus miles — there’s a start and a finish,” she says. “If we knew when this is going to end, that would bring us a great deal of structure. But we don’t have that right now, which is very hard for the human psyche.”
“When something throws us off, we try to problem-solve so we can get back into some type of regulation. But what’s happening here is the need for a reasonable level of predictability has really been threatened. There isn’t a definitive model that can lead us to know exactly how this is all going to play out” according to Brattleboro Retreat psychologist Dr. Jilisa Snyder in Vermont. The news cycle has placed so much emphasis on the mounting number of cases and the death rate. “A lot of people are in pain already,” Snyder says, “and this situation is very, very psychologically challenging.” It is recommended that you limit the amount of television news to 1 hour every morning, noon, and night. Dr. Snyder was interviewed by Kevin O’Connor in the VT Digger News site on March 28, 2020.
Ostensibly, stress has the capacity to change this normal resting heart rate and slowly raise our levels making it difficult to truly relax. In the long term, external stress can change our heart functioning including hypertension and cardiac arrhythmia and put us at risk for cardiovascular illness including heart attack and stroke. Lifestyle changes are necessary to avoid long-term health problems from stress. Mindfulness includes deep, regular breathing, guided imagery, and progressive relaxation. It is being introduced in some public schools so that it may become part of the coping mechanisms used by kids when stress sets them off – as it undeniably will do.
___________________________
References
O’Connor, K (2020) A Vermont therapist’s tips for balancing life in unsettled times. VT Digger Healthcare, March 28, 2020. Taken April 5, 2020.
VBSR Offers Webinar Series on Coronavirus Response Resources for Businesses https://vbsr.org/news-item/vbsr-offers-webinar-series-on-coronavirus-response-resources-for-businesses/
Sefton, M (2017) Chronic stress: The unbridled malignancy that affects us all. Blog post: https://wordpress.com/post/concussionassessment.wordpress.com/2785 taken April 5, 2020.
Photo credit cottonbro on Pexels.com
Australian TV: “Ask the Doctor” looks at a clock first published here
The clock drawing has become something of a cult following. It is curios and fun to look at the drawings produced by ordinary individuals. Most do very fine but some have difficulty on the task. I have published dozens of clocks in these pages and was approached by the producer of the Australian TV program “Ask the Doctor” if they could use one of the clocks I published. There are no defining elements that might expose the confidentiality of the patient in the show. I have been given permission by the producer to show the piece that was aired on Australian TV over a year ago. It is a show on Alzheimer’s Disease and is quite interesting.

Territorial Aggression seen in Traumatic Brain Injury

This is a case study of a 30-year old who was severely injured in a motorcycle crash nearly 6 months ago. He is aggressive and highly protective of his personal space. In terms of recovery from TBI, six months is not a long time, but this young man has more potential than therapy he will let us provide. He is easily angered and often physically threatening. Territorial aggression is a term that evolves from the animal behavior literature and has to do with the normal reaction of animals to threatened encroachment experienced to the enclave they claim as their own. It could be a tract of land, a small expanse of forest, or even a single tree. Animals guard their piece of the forest and often exhibit aggression associated with encroachment of that territory. “A territory is a defended space, and that defense is what distinguishes it from any other use of space” according to Breed and Moore, 2012 in Animal Behavior.
The ANS functions as the brain and body’s alarm system signaling the need for fight-flight activation. When this system is damaged due to traumatic brain injury the recovering subject can have wild swings of autonomic arousal such as elevated heart rate – patients sometimes chug along at 140-160 while autonomic storming. Sefton, 2018
Some believe that territoriality has evolutionary value for preservation of the species and is frequently seen in animals who are parenting (Breed and Moore). Its presence in human beings is somewhat conjectural at best. However, behavior change including increased restlessness, agitation, and aggression is seen in human beings during recovery from traumatic brain injury and it is plausible that under some conditions such as premorbid personality factors and functional changes due to severe brain injury, that territorial aggression may be present.
As just described, the patient is 30-years old. He sustained a TBI in September 2019 resulting from a motorcycle crash. His motorcycle struck the rear of a farm tractor in a rural county here in Massachusetts. He was brought to the trauma center with a Glasgow Coma Scale of 3 and spent the next 4 weeks in a coma or minimally conscious state before being transitioned to rehabilitation. He was not expected to survive but underwent an emergency craniectomy due to potentially life ending edema in his right parietal lobe. This involves the surgical removal of a portion of the skull. The computerized tomography scan (C-T) of his brain showed severe areas of bleeding and diffuse injury. He also sustained multiple fractures to his upper extremities and face. Once admitted to rehab, he remained in a somnolent, minimally conscious state for another 4 weeks. During the time following his admission he experienced episodes of autonomic storming that suggests that his fear reaction was on overdrive. When the lower brain centers are damaged they often run amok raising blood pressure, elevating heart rate, motor restless behavior, sleeplessness, and excessive sweating.
I am a neuropsychologist working at a rehabilitation hospital in Massachusetts where this man was sent to recover. We see over 200 patients annually with traumatic brain injury. Many are the result of motor vehicle accidents or falls of one kind or the other. We have an excellent medical, nursing, and rehabilitation staff of caring personnel.
The patient had major bleeding in his brain including both subdural hematoma and subarachnoid hemorrhages. The surgical removal of part of his skull was undertaken because of herniation in the left hemisphere that is often a sign that intracranial pressure has built up in the cranial vault. This very likely saved his life. The left parietal portion of his skull was put into storage and has yet to be reinserted. He had a contre coup injury to right temporal lobe of his brain as shown by the imaging conducted at the trauma center. There was significant damage of his orbital frontal cortex that are at work in processing the reward value of stimuli he feels and is linked to medial brain structures and pathways to the amygdala. The amygdala is the primary center deep within the brain for threat assessment and the primitive fear response. It also plays a role in attaching day-to-day experience to memory for recall later on that has modulatory impact on primitive drive behavior.
In animals, territorial aggression is often part of the scent marking behavior seen in males who are seeking dominance or alpha-male status within a territory. Social encounters between dominant males frequent become aggressive when one male’s territory becomes threatened by a perceived intruder. Territorial aggression is decreased in nonbreeding season and may be linked to changing levels of sex hormones and neurosteroids in many animals, including the frog, fish, and sparrow (Pradhan et al., 2010) in Wingfield (2016). So how does this relate to our motorcycle crash victim? Underlying personality plays a big role in initial behavior during the transition from minimally conscious to restless and agitated.
Past Social History
The patient was described as socially isolated as a young man. He had a history of criminal behavior starting as a child. On the day of his accident he was trying to pass a slow moving farm tractor on the right side just as the tractor was turning right. He was incarcerated in prison for a number of years for narcotic sales so his behavior resembled that of an inmate. He was not a heavy drug user but family has said he enjoyed marijuana. He was is “special schools” from the age of seven years old but his father did not know specifically why. He is thought to have poor social skills and a suspicious mistrust of authority. He had a few friends who visited from Western, MA. We anticipated his resistance and aggressive behavior but have found very little that served as rewards for him. He seemed to want no personal attention from any of the staff, he watched little or no TV, and was not interested in a game system available to him. His entire behavior was one of avoidance of intrusion into his personal space. We assumed that pain in his left knee played a big role.
Behavior changes is often associated with limbic system damage in patients exhibiting both reactive and non-purposeful anger. In the case of this one human being, by outward appearance, his internal motivational state has been solely to defend his territory or personal space measuring just his bed and approximately 6-12 inches in the perimeter. Normally we would see patients slowly awake from coma and gradually exhibit an awareness of what has happened to them and why they are in the rehabilitation hospital. George Prigatano, Ph.D., at the Barrow Brain Institute in Phoenix, described this gradual re-acquisition of conscious awareness as an element of higher cognitive functioning, an internal mental representation of an event or interaction, and initiation of some primary response. In lower level cases such as this one, there is very limited initiation of responses but clinicians believe that responses that are spontaneously observed are based expressed archetypes of basic personality that are largely automatic (Prigatano, 1999). The patient has a loss of appreciation for a sense of ‘self’ as opposed to ‘other’ and its social representation in the treatment he receives daily.
Efforts to establish a trust by giving him control over his “territory” were undertaken. I suggested a consistent team and consistent timing. None of the team seemed to imprint upon him. We utilized the Aggressive Behavior Rating scale to measure the behaviors that were present on a daily basis. The ABRS is a 14-item scale that uses a likert-type 1-4 point rating system where 1 is the absences of a behavior and 4 is an almost constant expression of the behavior. The ABS scale is used for measuring verbal and physical abuse, socially inappropriate behavior, and resisting care (Perlman and Hirdes, 2008). His weekly average went from 29 to 21 to 18. Over time, he became more cooperative with one male aide who was straight forward and consistent. The aide went in to the patient’s room and told him in a non-threatening way what he could expect and when he could expect it. In this way, he was quite good at establishing a quasi-cooperative routine for personal hygiene when he was incontinent. With most other people on the brain injury team he was coiled and ready to strike whenever his treatment refusal was ignored and the team pushed on. His medications have been adjusted with the primary pharmacology being depakote for mood stability. The target of keeping his level on the higher end of normal between 90-100.
The patient is not able to be formally tested due to on-going aphasia. His yes/no reliability has improved especially when it came to his physical condition e.g. do you need to go back to bed?, are you in pain? His eye contact is better and we can now see his blue eyes. His social information processing was seemingly apathetic to conventional cues, reward, and social reciprocity as he has recovered. He exhibited sadness and was tearful on occasion. He has expressive aphasia and can follow some simple commands but rarely does so. His verbal output is aphasic word salad – often perseverating. He seems to have broad somatosensory deficits including tactile defensiveness, especially when auditory stimuli are pronounced. He has visual sensitivity to light and prefers to have all outside curtains closed and his bed kept in the dark. His gustatory system is presumably functional as he eats everything that is given to him and has gained a good deal of weight. He has some preferences in his daily dining routine that are accommodated as much as possible. At one point in the treatment, we made an effort to pair food delivery with being out of bed and dressed for the day with very limited success. He became frustrated with having the food tray out of arm’s reach that he was able to kick out striking the tray sending it across the room in defiance. Olfaction has not been measured with unequivocal precision. He is not cooperative with sensory testing.
He appears to have only avoidance as his primary behavioral motivation. He becomes aggressive in an effort to avoid treatment demands even as basic as sitting in his wheelchair or rolling in bed so as to be cleaned. AT one point he had a grip on my tie that was impossible to break. I calmly said to him that it was my favorite tie and “I would appreciate that he not rip it off my shirt.” His treatment will continue for the foreseeable future. The coronavirus has put a chink into his recovery whereby his routine has been altered somewhat. He has no symptoms and is not considered at risk. His father is dutiful in his daily update calls and has stood by him – now virtually. His aggression has diminished and our data collection has demonstrated a downward trend in his behavior. We are hopeful that he will continue to clear and remain engaged in his treatment. I have seen him sing and reach out for fist bumps. Unfortunately, the fear of Covid-19 does not allow us this celebratory display of praise, that we all so much want to share.
___________________________
References
Wingfield, J Ecophysiological Studies of Hormone–Behavior Relations in Birds: Future Challenges in a Changing World. Volume 2, 2017, Pages 321-345.
Sefton, M (2018) Autonomic Storming. Blog post: https://concussionassessment.wordpress.com/?s=storming, taken March 30, 2020.
Perlman, C and Hirdes, J (2008) The Aggressive Behavior Scale: A New Scale to Measure Aggression Based on the Minimum Data Set. Journal of the American Geriatric Society. https://doi.org/10.1111/j.1532-5415.2008.02048.
Breed, M and Moore, J (2012) Animal Behavior. Academic Press. Boston.
Prigatano, G and Schacter, D (1991) Awareness of deficits after Traumatic Brain Injury: Clinical and Theoretical Issues. Edited by Chair Section of Clinical Neuropsychology George P Prigatano and Daniel L. Schacter, University of Arizona.
Clock of the week
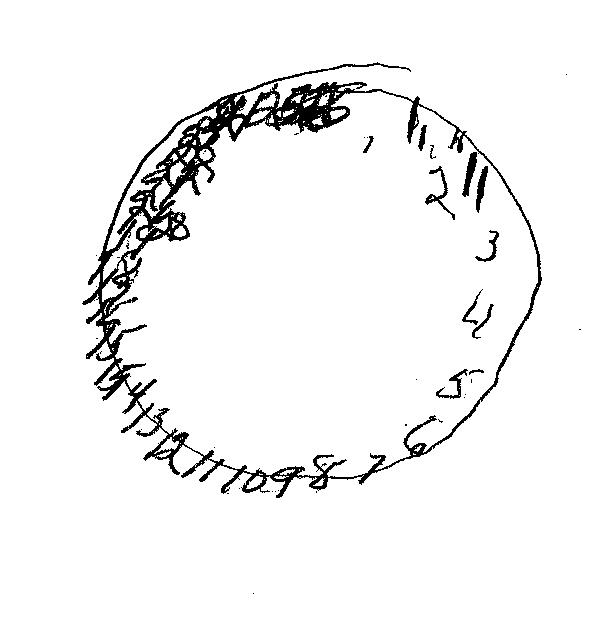
One of the clocks previously published here at the Concussion Assessment and Management blog was chosen by the Australian Broadcast Company as an illustration of how dementia effects cognition in older Australians. I was contacted 6 months ago by the show’s producers. I think they struck by the simplicity of the task and the variety of responses we see clinically. The program called “Ask the Doctor” is a weekly broadcast in Australia about varying health concerns faced by the aging population down under. Like here in the United States, health concerns including Alzheimer’s dementia are covered by the producers of the show. I was sent a link to the show and have asked permission to post the broadcast that contains the clock drawing. It shows how important it is to understand cognition and dementia. I will post a link to the You Tube video of the original clock drawing below.
The Clock of the Week is drawn by a 65-year old male who is struggling from the effects of respiratory failure and its impact on debility. He has a tracheostomy tube in place and cannot speak. He communicates using gesture such as when he is thirsty. He is irritable and was eager to write to me when given the chance.
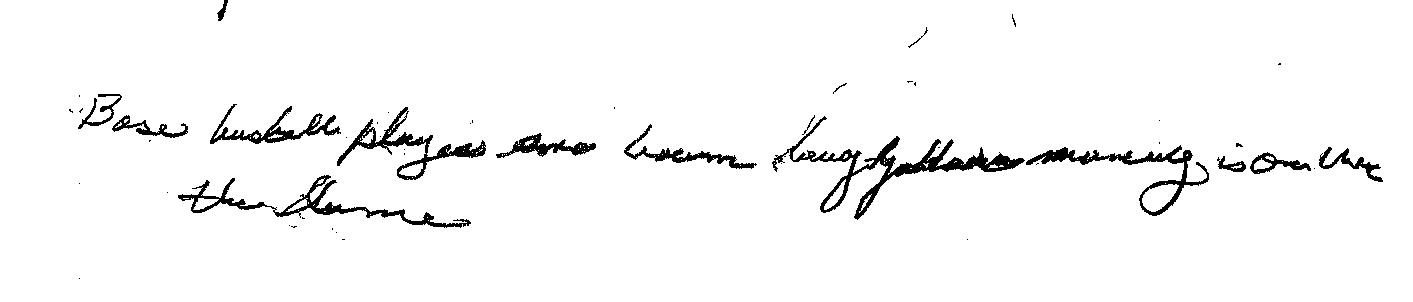
Here is a sample of his written language output. He was asked to write the sentence “Baseball players are tough”. You can see from the writing above that he put forth his best effort but still has a way to go to use written output as a bona fide communication modality. In cases such as this the clinical team is asked to use Yes/No inquiry to assess his language and for gaining deeper understanding of the physical and emotional adjustment through which this man is going. He is participating in treatment in spite of his frustration, anxiety, and thirst. Once he is able to swallow he will be given a hospital diet by mouth. Until then he receives full nutrition via a gastronomy tube in his stomach.
Here is a copy of the You Tube video that depicts the clock that was used on the Australian Broadcast Company “Ask the Doctor” program that was broadcast in October, 2018. In Australia there are thousands of new cases of dementia diagnosed weekly. Watch the video and share it.
Sports specific recovery from Concussion

-
Body checking starts at age 11 in most sanctioned ice hockey programs PHOTO: Mike Sefton
October 9, 2018 Cognitive and emotional symptoms often occur when an athlete sustains a concussion. Individual sports have somewhat different trajectories when it comes to recovery – sometimes because of the nature of the sport and sometimes unique to the athlete and his or her emotional predisposition. Ice hockey is a high speed collision sport. Many athletes play the game on a year round basis chasing a dream of collegiate or professional status. Ice hockey has a high degree of collision-related concussions according to the National Council on Youth Sports.
Contrary to current beliefs, even currently healthy youth hockey players reported higher persisting psychological symptoms among those with a history of concussion. Psychological sequelae appeared unique to a history of concussion as athletes with a history of musculoskeletal injuries did not present with the same persisting psychological symptoms. A study in Pittsburgh looked at the incidence of concussion among younger and older adolescent players from elite hockey programs. They found a higher rate of concussion among younger players. In a post last month I presented the notion that size matters when it comes to elite (younger) athletes playing against older and more physically developed athletes. Concussions tend to be both more frequent and more long lasting.
As with any risk-reward scenario, decisions about physical risk must be considered when a player is invited to play up against older and more developed players. I have seen freshman football players competing at a varsity level and be severely harmed both physically and psychologically by the shear difference in size and strength. Younger athletes are often misinformed as to the physical demands of a varsity sport and wrongly believe they are athletic failures and weak unless they play through their injuries – including concussion according to Sefton, 2018.
In 2016 the majority college ice hockey player spend one to two years in junior hockey (ages 17-21) allowing them to continue their physical development prior to entering college hockey. This includes not only Division I scholarship programs but Division II and Division III programs as well. Very few natural freshmen play college hockey at 18 years of age unless they are highly gifted athletes. Even these players are coached and managed by trainers with ongoing development programs, weight training, and nutritional support to enhance upper body size and strength. Michael Sefton, 2016
Even though sport concussion is considered a unique subset of MTBI, results suggest that a smaller percentage of youth may be more prone to psychological sequelae following concussion. This means that not all concussions are created equal. Along with colleagues across the country I have been saying this for over 20 years. There is a literature on elite ice hockey players and a co-occurring mood disorder that needs to be addressed as they heal.
When I first started taking an interest in MTBI, also called concussion, physicians did not believe that someone sustained a brain injury unless there was a bonafide loss of consciousness. This remains one of the greatest myths in brain injury rehabilitation and I still hear from people that a son or daughter has a concussion “but he did not get knocked out” as if that minimizes the significance of the injury they sustained. Finally, I am still getting significant push back from the parents of children who are diagnosed with multiple concussions. The recovery from concussion two or three is not the same trajectory as the first. Many wonder why their child hasn’t bounced back like they did the first time around. And common to second concussion irritability and other mood-related changes are common.
I suggest to parents expect the unexpected and try not to attribute changes in school functioning to laziness alone. Plan on working with the school-based support team and athletic trainer as you return to learn and return to play. Most elite programs offer emotional support for athletes suffering with the effects of concussion. Many feel isolated or marginalized because they may appear normal and walk and talk just like other members of the team. Athletes recovering from concussion are at higher risk of second concussion if they return to play before their injuries heal. This takes 7-21 days on average.
The Pittsburgh study, published in Pediatrics in 2016, revealed that the population of ice hockey players they studied had a higher preponderance of players who had sustained one or more concussions. This is what I experienced in looking at junior level ice hockey (typically aged 16-20 years) teams a few years ago. I was surprised when I asked how many had sustained a prior concussion and most all the players raised their hands. Fighting is first allowed in this level of play and sometimes becomes a handicap for players with sites set on collegiate play. In many cities across the country junior hockey is the only show in town. Some cities in the mid-west actually televise games and report scores on local sports programs.
Remember no two concussions are the same. Sports all have their return to play protocol that begins with recognizing the importance of controlled exertion in the setting of concussion and recovery.
Sefton, M. (2016). Body Checking in Hockey: When size matters. Blog post: https://concussionassessment.wordpress.com/2016/03/14/body-checking-in-ockey-size-matters/ Taken October 9, 2018
National Council on Youth Sports. Report on trends and participation in organized youth sports. Available at: www.ncys.org/publications/2008-sports-participation-study.php. Published 2008. Accessed March 17, 2015
Kontos, A. et.al. (2016) Incidence of Concussionin Youth Hockey Players http://pediatrics.aappublications.org/content/early/2016/01/07/peds.2015-1633#ref-5 PEDIATRICS Volume 137, number 2 , February 2016 :e 20151633 Taken October 9, 2018
Clock of the Week: 8-15-18