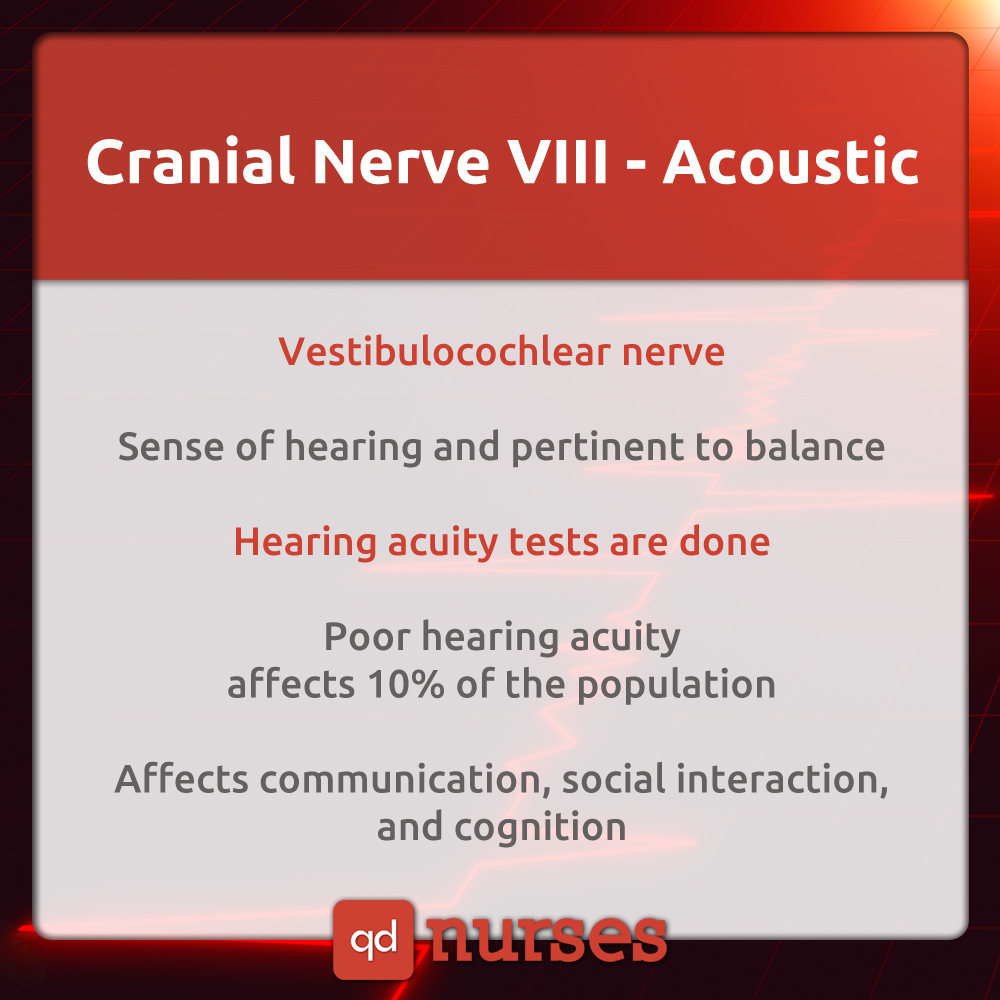
 WESTBOROUGH, MA July 16, 2018 I have recently been taking care of a couple of men who have experienced significant hearing loss as they aged. The loss of any sensory system contributes to a significant change in independence and satisfaction in life. In this systematic review and meta-analysis of 36 epidemiologic studies and 20 264 unique participants, age-related hearing loss was significantly associated with decline in all main cognitive domains and with increased risk for cognitive impairment and incident dementia. Increased risks for Alzheimer disease and vascular dementia were not statistically significant.
WESTBOROUGH, MA July 16, 2018 I have recently been taking care of a couple of men who have experienced significant hearing loss as they aged. The loss of any sensory system contributes to a significant change in independence and satisfaction in life. In this systematic review and meta-analysis of 36 epidemiologic studies and 20 264 unique participants, age-related hearing loss was significantly associated with decline in all main cognitive domains and with increased risk for cognitive impairment and incident dementia. Increased risks for Alzheimer disease and vascular dementia were not statistically significant.
“Hearing loss may have a profoundly detrimental effect on older people’s physical and mental well-being, and even health care resources,” says senior study investigator and Johns Hopkins otologist and epidemiologist Frank Lin, M.D., Ph.D.
“Our results underscore why hearing loss should not be considered an inconsequential part of aging, but an important issue for public health,” says Lin, an assistant professor at the Johns Hopkins University School of Medicine and the university’s Bloomberg School of Public Health. According to Lin, as many as 27 million Americans over age 50, including two-thirds of men and women aged 70 years and older, suffer from some form of hearing loss.
“Dr Frank Lin says social isolation resulting from hearing loss may explain the physical and mental declines – as well as the cognitive deficits – that afflict older adults. This, in turn, may lead to more illness and hospitalization, he says. His team already has further research under way to see if treating hearing loss with counseling and hearing aids can reduce people’s risk of cognitive decline and dementia”.
Tinnitus is sometimes associated with hearing loss. Tinnitus is also known as ringing in the ears and is described by many as a constant high pitched sound or whistling noise. It is sometimes attributed to “trauma” from years of employment or working in an industry that required no hearing protection.
I have begun using a new protocol in my biofeedback session for those most bothered by tinnitus. Neurofeedback is a non- invasive neuromodulation technique which records a subject’s neuronal activity, extracts relevant aspects of brain processes by means of real time signal processing and returns feedback to the subject as visual or auditory stimuli. The aim of neurofeedback is to change behavioral traits or medical conditions associated with altered neural activity as demonstrated for chronic tinnitus.”
“Subjective tinnitus has been described as the constant perception of an auditory sensation that does not correlate to any external acoustic stimulus (Stouffer and Tyler, 1990). It can be perceived as either pitch or noise-like sound and its perception may be unilateral, bilateral or spread out in the whole head (De Ridder et al., 2014b).”
Loughrey DG, Kelly ME, Kelley GA, Brennan S, Lawlor BA. Association of Age-Related Hearing Loss With Cognitive Function, Cognitive Impairment, and Dementia A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg. 2018;144(2):115–126. doi:10.1001/jamaoto.2017.2513
Güntensperger D, Thüring C, Meyer M, Neff P and Kleinjung T (2017) Neurofeedback for Tinnitus Treatment – Review and Current Concepts. Front. Aging Neurosci. 9:386. doi: 10.3389/fnagi.2017.00386
De Ridder, D., Fransen, H., Francois, O., Sunaert, S., Kovacs, S., and van de Heyning, P. (2006). Amygdalohippocampal involvement in tinnitus and auditory memory. Acta Otolaryngol. 126, 50–53. doi: 10.1080/03655230600895580
Stouffer, J. L., and Tyler, R. S. (1990). Characterization of tinnitus by tinnitus patients. J. Speech Hear. Disord. 55, 439–453. doi: 10.1044/jshd.55 03.439



 WESTBOROUGH, MA July 16, 2018 I have recently been taking care of a couple of men who have experienced significant hearing loss as they aged. The loss of any sensory system contributes to a significant change in independence and satisfaction in life. In this systematic review and meta-analysis of 36 epidemiologic studies and 20 264 unique participants, age-related hearing loss was significantly associated with decline in all main cognitive domains and with increased risk for cognitive impairment and incident dementia. Increased risks for Alzheimer disease and vascular dementia were not statistically significant.
WESTBOROUGH, MA July 16, 2018 I have recently been taking care of a couple of men who have experienced significant hearing loss as they aged. The loss of any sensory system contributes to a significant change in independence and satisfaction in life. In this systematic review and meta-analysis of 36 epidemiologic studies and 20 264 unique participants, age-related hearing loss was significantly associated with decline in all main cognitive domains and with increased risk for cognitive impairment and incident dementia. Increased risks for Alzheimer disease and vascular dementia were not statistically significant.


